You may have looked at the title of this blog and thought to yourself, what in the world is peri-partum depression?! Educational campaigns directed at both physicians and the public have done a great job of increasing awareness about post-partum depression and the so-called “baby blues.” These efforts have been so successful in fact, that many obstetricians automatically screen women for depression at their 6-week after delivery checkup. But did you know that of the 15 percent of pregnant women who develop depressive symptoms, half of those develop their symptoms during pregnancy, not after? Hence, the title. The prefix peri- means “around” in Latin. Peri-Partum depression is any depression that develops during or shortly after pregnancy. Rather than narrowing the focus to depression that starts after delivery, screening for peri-partum depression allows us to identify women who could benefit from additional support, counseling, therapy, medications and/or whatever combination of all of those things, to reduce depressive symptoms both during and after the pregnancy.
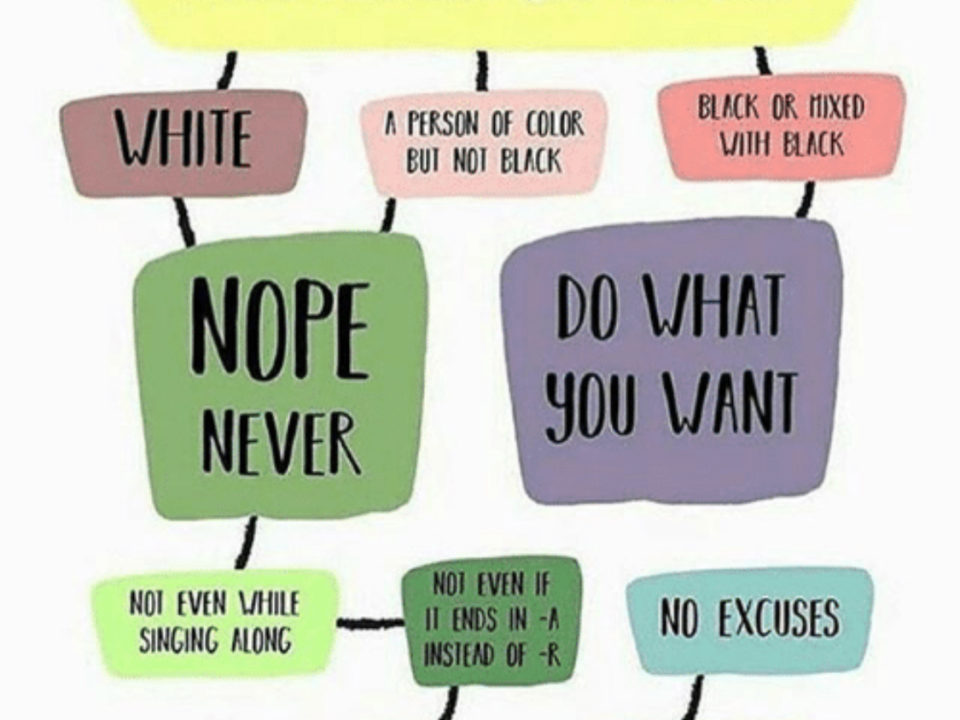
So, we tackled the first part of the title – Peri-Partum Depression. How about the second part? Under-Recognized and Under-Treated. Unfortunately, both are so true. While there has been a much-needed growth in awareness around peri-partum depression, a lot of depression in pregnant women is still going unrecognized. As concerning, is that even when the depressive symptoms are recognized, about 1/3 of those women never receive additional support or treatment. We have got to get our hands around this problem! Untreated depression in pregnant women has been irrefutably linked to premature labor, smaller birth weight babies and poorer maternal health. Depressive symptoms after delivery can lead to difficulty with emotional attachment between the mother and infant. None of those outcomes, are what we want. So why are depressive symptoms going under-recognized and under-treated? The answer is – for the same reason other mental health symptoms go under-recognized and under-treated: stigma and lack of access to care likely being the top 2 reasons on the list. As stigmatized as mental health symptoms are in general, depressive symptoms either during or after pregnancy is super stigmatized. I mean really, the most miraculous, amazing thing is happening to you, right? How in the world can you tell people you feel sad, hopeless, overwhelmed and maybe even suicidal?
Now here is the last curve ball -- did you know that men can also develop post-partum depression? Estimates vary, but somewhere between 1 in 10 and 1 in 4 men develop depressive symptoms after the birth of a child. Whatever the real number -- it is significant. Depressive symptoms in men can lead to difficult attaching to infants, marital problems and worsening of depressive symptoms in mothers. So again, we have got to get our arms around this issue.
What we have to do is make it possible for women and men to tell us that they are exhausted, sad, hopeless, overwhelmed, having trouble connecting to the baby. And this challenge is not just for OB doctors – this challenge is for all of us – friends, family, co-workers, physicians – all of us! We have to reduce the stigma of identifying the depressive symptoms, and we have to create availability of supports that can help once the symptoms have been identified.
If you or someone you know is experiencing symptoms of peri-partum depression, Post-Partum Progress and Post-Partum Men are great organizations that may be able to help you get linked to support.